Understanding Arthritis Causes, Symptoms, and Treatments

Understanding Arthritis: Causes, Symptoms, and Treatments
Arthritis is a pervasive condition affecting millions of middle-aged adults in the United States, with the CDC reporting that 21.2% of adults aged 18 and older—approximately 53.2 million Americans—live with diagnosed arthritis .18 .20. For those aged 40–55, arthritis often marks the beginning of chronic joint discomfort, impacting daily productivity, physical independence, and long-term health outcomes. This article synthesizes current medical knowledge, lifestyle strategies, and treatment advancements to empower middle-aged individuals with actionable insights for managing arthritis effectively.
The Biological Foundations of Arthritis

Defining Arthritis and Its Common Forms
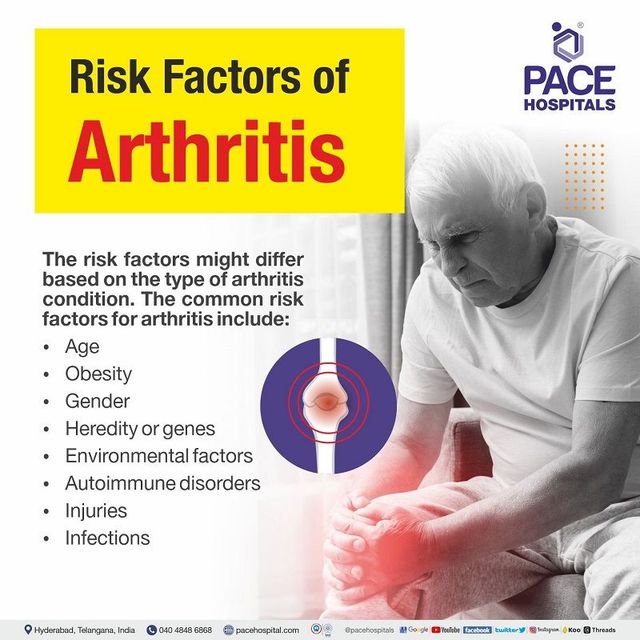
Arthritis encompasses over 100 conditions characterized by joint inflammation, pain, and stiffness. The two most prevalent types are osteoarthritis (OA) and rheumatoid arthritis (RA). OA, often termed “wear-and-tear” arthritis, results from the gradual breakdown of cartilage that cushions joints, leading to bone-on-bone friction .5 .17. It predominantly affects weight-bearing joints like knees, hips, and the spine. RA, an autoimmune disorder, occurs when the immune system mistakenly attacks the synovium—the lining of joints—triggering inflammation, cartilage erosion, and bone damage .5 .19. Other forms include psoriatic arthritis (linked to psoriasis) and gout (caused by uric acid crystals) .19.
Middle-aged adults are particularly susceptible to OA due to cumulative joint stress from decades of activity, while RA often emerges earlier but progresses silently .20. Notably, 40% of adults aged 45–64 report arthritis, with women 1.3 times more likely to develop it than men .18 .20.
Causes and Risk Factors in Middle Age
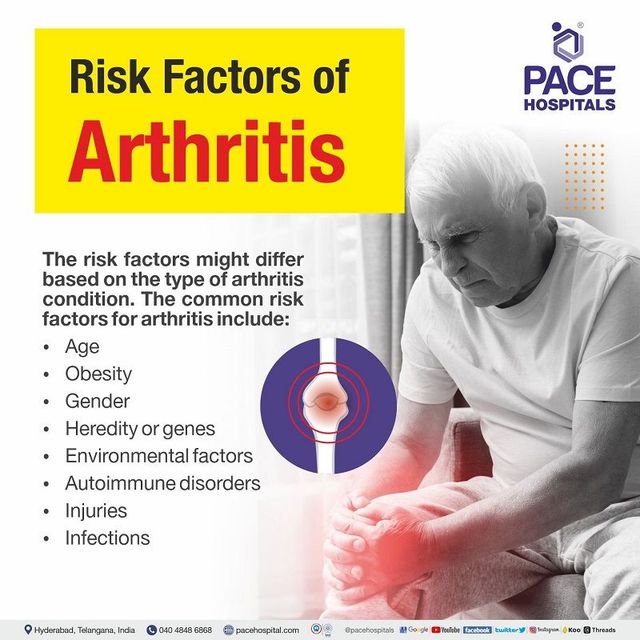
Biological and Environmental Triggers
The development of arthritis in midlife is multifactorial:
-
Age-Related Cartilage Degradation: Cartilage loses elasticity and repair capacity after age 40, accelerating OA .5.
-
Genetic Predisposition: Family history increases RA risk, particularly in individuals with specific HLA-DR4 gene variants .11.
-
Obesity: Excess weight strains joints and promotes inflammatory cytokines; 56.8% of obese adults over 65 have arthritis .18 .14.
-
Prior Joint Injuries: Fractures or ligament tears predispose individuals to post-traumatic OA .5.
-
Occupational Hazards: Repetitive motions in jobs like construction or nursing contribute to joint overuse .14.
-
Lifestyle Factors: Smoking doubles RA risk by triggering autoantibodies, while excessive alcohol consumption exacerbates inflammation .3 .14.
Socioeconomic disparities also play a role: adults with household incomes below the poverty line face 36% higher odds of arthritis due to limited access to preventive care and healthier lifestyles .14.
Recognizing Symptoms and Seeking Diagnosis
Early Warning Signs
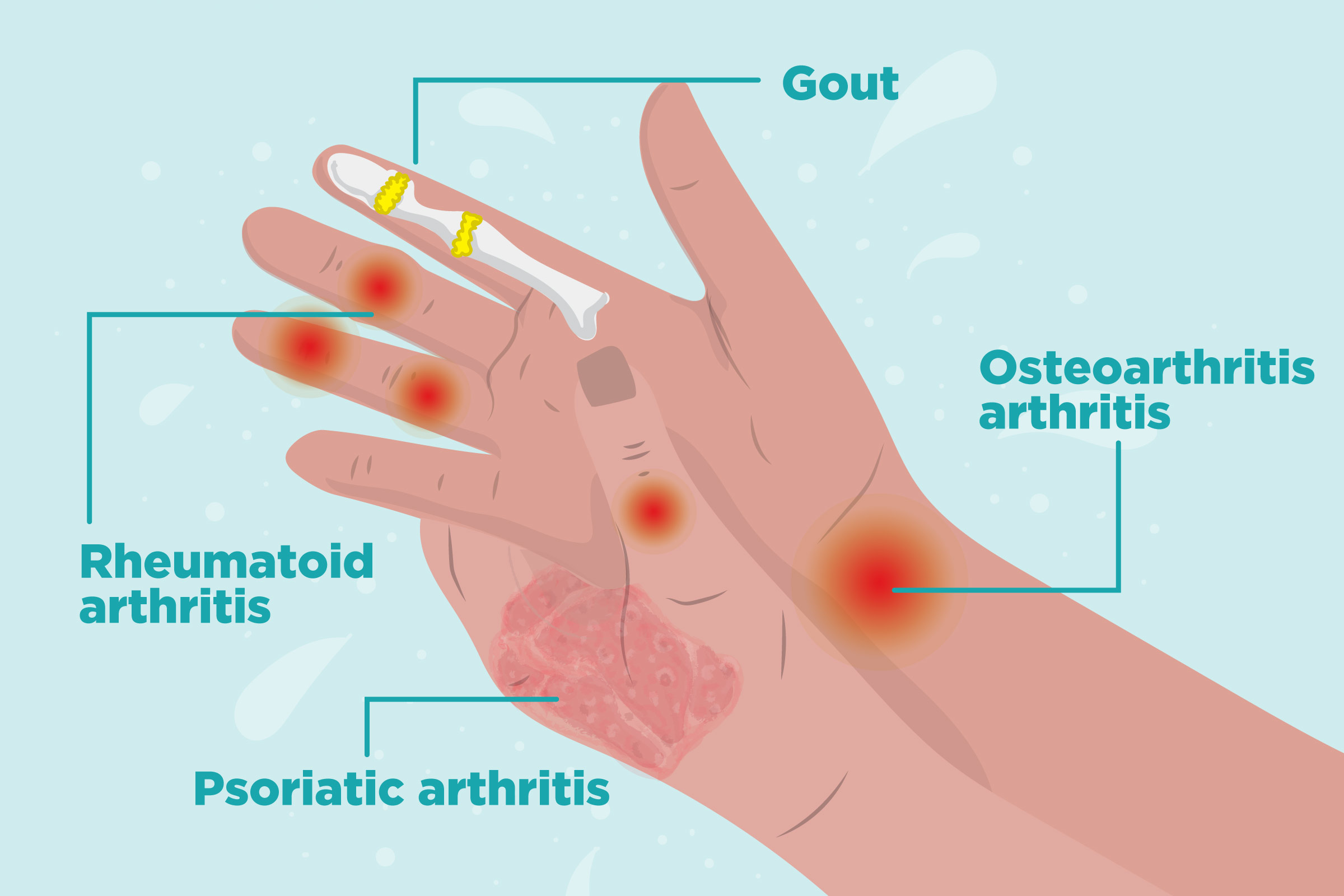
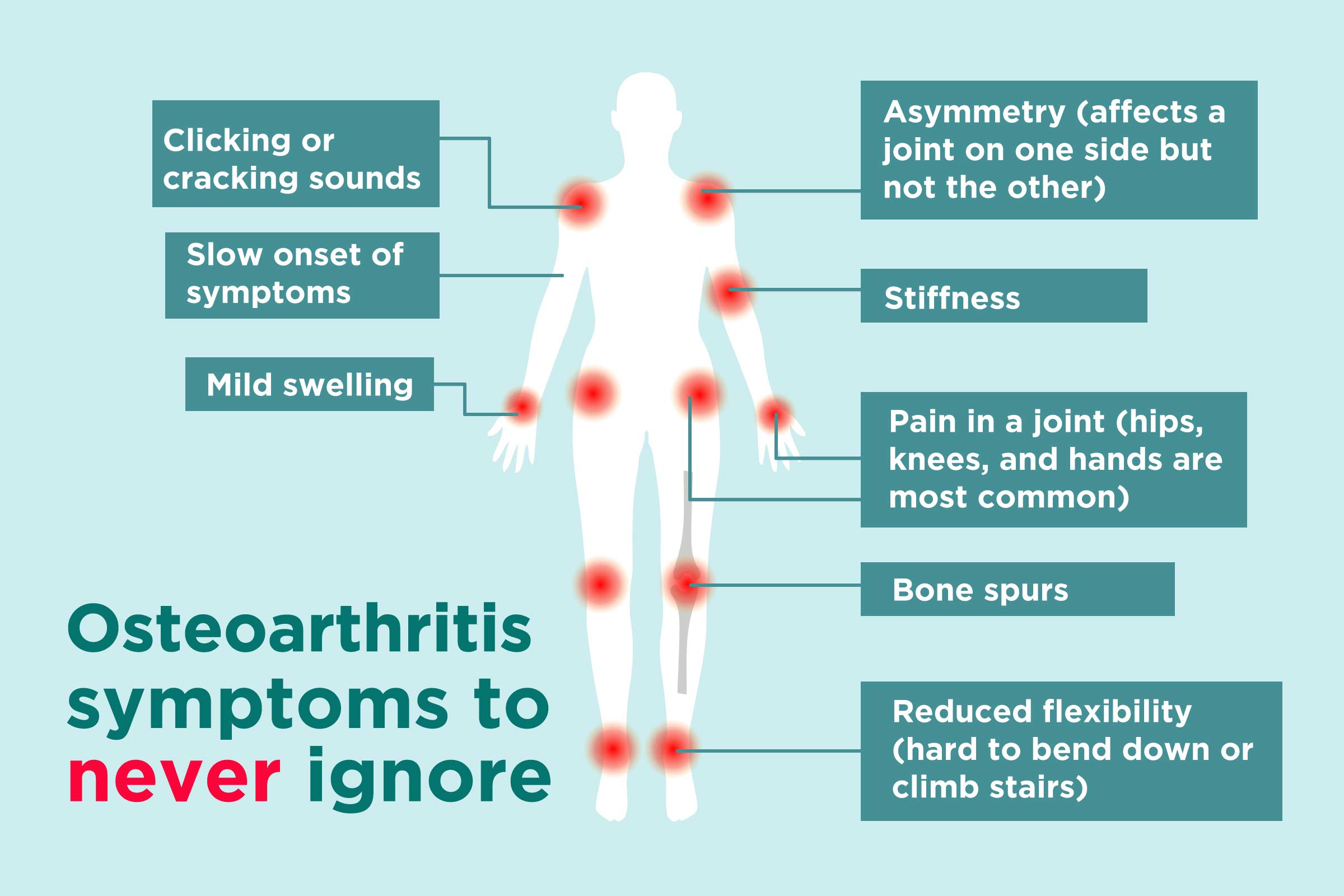
Arthritis symptoms often begin subtly but worsen over time:
-
Joint Pain and Stiffness: Morning stiffness lasting >30 minutes suggests RA, while OA pain worsens with activity .17 .19.
-
Swelling and Redness: Inflammation in RA causes warm, tender joints, whereas OA swelling is typically mild .5.
-
Reduced Mobility: Difficulty climbing stairs or gripping objects signals joint damage .2 .12.
-
Systemic Symptoms: RA may involve fatigue, fever, or weight loss due to systemic inflammation .5.
Diagnostic Pathways
Early diagnosis prevents irreversible joint damage:
-
Clinical Evaluation: Physicians assess medical history, symptom patterns, and perform physical exams to check for tenderness or deformities .17.
-
Imaging: X-rays reveal cartilage loss in OA, while MRIs detect synovial inflammation in RA .







